The cure for cancer might have been inside us all along – our own immune system. The trick is to give it a boost to find and destroy those rogue cells, and that’s the focus of the field of immunotherapy. To that end, a new hydrogel has been developed that can be injected directly to the site of a tumor, where it stays to slowly release its payload of immunotherapy drugs for longer.
Put the two into a ring, and the immune system will win every round against cancer. To give itself a fighting chance, the Big C instead focuses its attention on stealth attacks, using a variety of tactics to evade detection by the immune system until it can grow strong enough to overwhelm the body.
Immunotherapy aims to swing the odds back into our favor, re-arming the immune system with new ways to detect and kill cancer cells. These techniques mainly involve extracting a sample of a patient’s T cells, genetically engineering them to attack tumors, and returning them to the body. Others may be able to stimulate the system with a single injection, akin to a cancer vaccine.
Cyclic dinucleotides (CDNs) are a type of drug sometimes used in immunotherapy treatments, usually administered through a simple injection. The problem is that the drugs end up being circulated throughout the body, which diminishes the concentration at the tumor site and results in them being flushed out of the body relatively quickly.
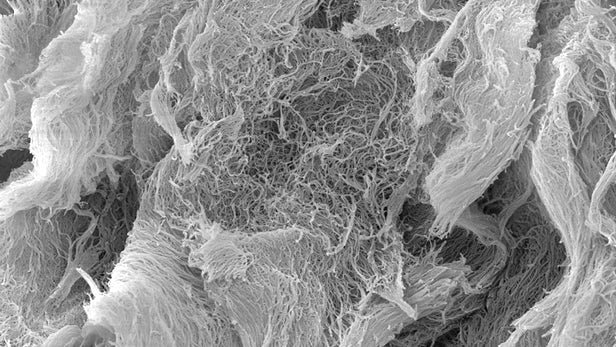
The new study, conducted by researchers at Rice University and the University of Texas Health Science Center (UTHealth), set out to keep the drugs in the right spot for longer. Rather than being contained in a liquid solution, the CDNs are loaded onto self-assembling multidomain peptide (MDP) hydrogels. These start off in a liquid form for injection, but once inside the body they quickly turn semi-solid, before degrading slowly over time. In the process, they release their cancer-killing CDNs more gradually and precisely. The team calls their creation STINGel.

“The normal approach to CDN delivery is simple injection, but this leads to very rapid diffusion of the drug throughout the body and reduces its concentration at the site of the tumor to very low levels,” says Jeffrey Hartgerink, lead researcher on the study. “Using the same amount of CDN, the STINGel approach allows the concentration of CDN near the tumor to remain much higher for long periods of time.”
The researchers tested the STINGel’s effectiveness in a series of lab tests, both in culture and in rodents. In the latter, the team divided rodents up into six groups of 10. One group received normal injections of CDN. Another was treated with control collagens on their own, while a third received those same collagens loaded with CDN. Another group received STINGel – containing CDN in an MDP hydrogel – while another received just the MDP without the CDN.
The team found that for the groups that were treated with liquid CDN and those treated with collagen and CDN, only one of 10 animals survived for 105 days. Among those treated with STINGel, on the other hand, six out of 10 survived that long. Better yet, even when the researchers implanted more cancer cells, this group managed to fight them off. This indicates that their immune systems had effectively learned to recognize cancer into the future – a promising start towards a potential “vaccine.”
“The MDP hydrogel provides a unique environment for the release of CDN that other gels just can’t match,” says Hartgerink. “The CDN we used in this study is currently in clinical trials. We think that our STINGel approach has the potential to significantly broaden the scope of this powerful immunotherapy drug to a larger range of resistant cancers.”