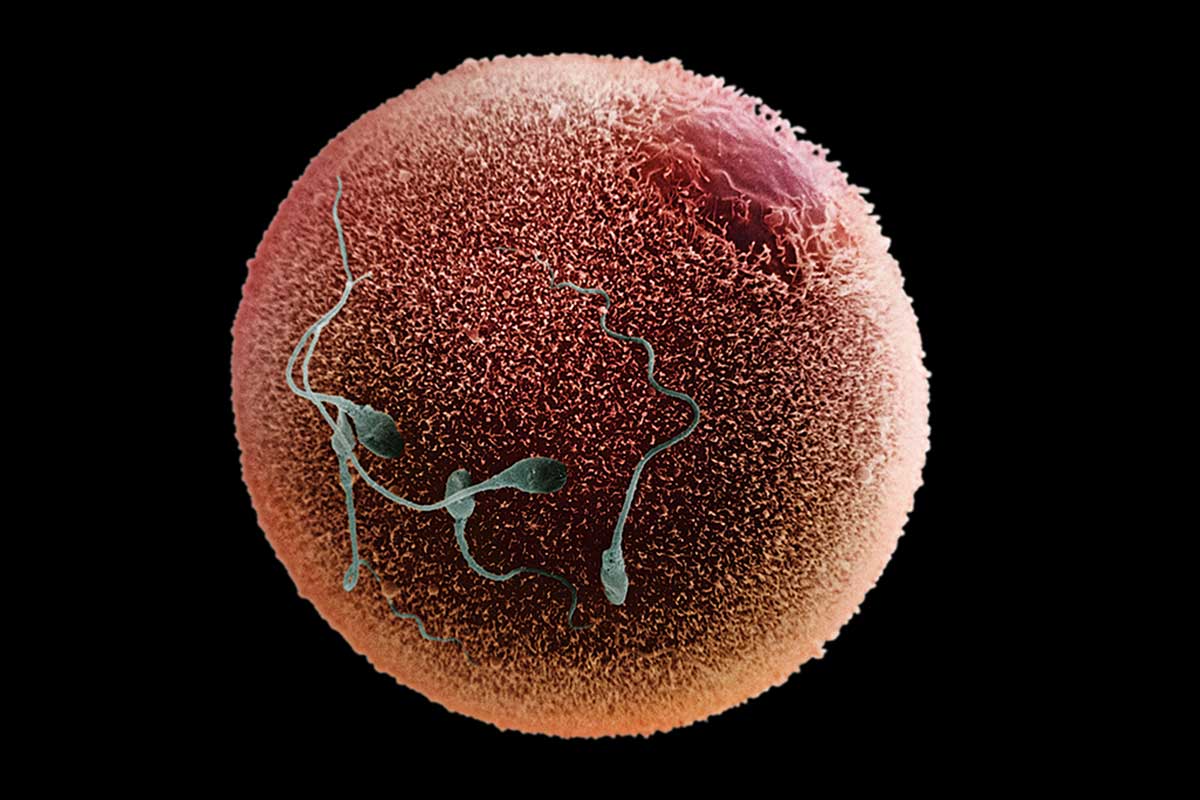
Human eggs have been matured from their most primitive state to full development in the lab for the first time. The resulting eggs are ready to be fertilised, and, if healthy, could in theory be used to advance IVF treatments as well as helping women who had cancer when they were young.
“It is really exciting,” says Michael Dahan at McGill University Health Centre in Montreal, Canada, who was not involved in the work. “It has the potential to improve treatment.”
Scientists have been trying to develop human egg and sperm cells in the lab for years, in order to better understand how these cells work, and to improve treatments for the growing number of infertile couples and individuals. But until now, they’ve only managed it in animals like mice.
“Working with mouse tissue is incredibly easy,” says Evelyn Telfer at the University of Edinburgh, who led the new work. “The composition of human tissue is quite different, and is not straightforward.” This is partly due to the presence of multiple supportive cells that surround the egg, making it more difficult to access and work with, she says.
Telfer’s team have overcome this hurdle by persevering with their technique for years, continually tweaking it to get the conditions right for egg growth. “We’ve been bullish,” says Telfer. In their procedure, the team start with tiny pieces of ovarian tissue, taken from 10 female volunteers during caesarean section surgery.
The team then look for what are called “primordial follicles” – small structures that each have the potential to release an egg. Women are thought to be born with all the follicles they will ever have. Most follicles remain inactive during a woman’s life, but some begin to grow in order to release an egg in ovulation. “In humans, they can sit there for 40 years before they start to grow,” says Telfer.
Fully mature
The primordial follicles are then placed in a nutrient-rich liquid, where they start to grow. There is no particular ingredient that kickstarts the growth, says Telfer. She believes that the act of chopping up the ovary is enough to activate development. This chimes with the findings of a Japanese group, who essentially chop up bits of women’s ovaries and re-implant them to improve their fertility.
Telfer and her colleagues then removed the individual eggs from each follicle, and focused on getting them to grow on their own to a size you would see at ovulation.
While some of the eggs failed along the way, a fraction continued to develop to a fully mature state. The team could tell these eggs were ready to be fertilised because they had undergone a key stage of cell division, in which the number of chromosomes is halved. The end result is a large egg cell with 23 unpaired chromosomes – ready to be combined with a sperm cell – and a much smaller sphere of cytoplasm containing the other chromosomes, which is known as a polar body. These tend to be broken down in a woman’s body.
Of the 310 primordial follicles the team started with, 87 survived the initial stage of the experiment. From these, the team were able to obtain 32 fully mature eggs. The whole process took between 21 and 22 days.
These eggs are technically ready to be fertilised with sperm. The team do not yet have a licence to do this, but have applied for one. If it can lead to healthy embryos, the technique could potentially be used in a range of fertility treatments.
Young girls with cancers often have pieces of their ovaries removed before they receive treatments that can damage their egg supply. The idea is to re-implant the tissue when the girls are older, and ready to start a family. But sometimes this isn’t ideal – the tissue might contain residual cancer cells, for instance.
Better IVF
Telfer’s technique could provide an alternative. If mature eggs could be developed from the ovarian tissue in the lab, these could be fertilised as part of IVF, allowing only the resulting embryos to be implanted.
In theory, the technique could also be used to improve IVF. At the moment, women who opt for IVF are given often gruelling hormonal treatments, which trigger the release of multiple eggs. These are then collected and fertilised with sperm in the lab. Sometimes the eggs might be too immature to use, says Dahan. In these cases, there’s a chance that the new technique could bring them up to scratch, boosting the total number available for IVF and increasing a woman’s odds of conceiving. “It’s something we could use to help develop [eggs] we would have had to discard in the past,” he says.
There are other potential benefits for IVF. If ovarian tissue can be used to obtain mature egg cells in the lab, then why not bypass hormonal treatments and egg extraction altogether? Surgery to remove a piece of ovary is invasive, and the risks wouldn’t be justified in most cases, says Dahan. But for women who are already having surgery, such as for endometriosis – a common cause of female infertility – this could be an option in the future, he says.
Before that, the team will have to be sure the eggs are healthy. While they appear fully matured, they aren’t identical to those released by ovaries. In particular, the polar bodies they produce are much larger than normal – at least twice the size, says Telfer.
This might be harmless, as the polar bodies are discarded anyway, but if the eggs are losing out on valuable cytoplasm – including the energy-providing compartments it contains – they might end up worse off as a result.
In the meantime, Telfer hopes the technique will help her and others understand more about how eggs develop, and what goes wrong in fertility disorders that lead to a lack of eggs, known as primary ovarian insufficiency. “There are several conditions in which women lose their eggs much earlier in life, or they don’t grow,” she says. “If we could understand the process… we could develop treatments for that.”